By IbogaHealth.org | April 2025 | Tijuana, Mexico
Abstract
Parkinson’s disease (PD) is a progressive neurodegenerative disorder with limited therapeutic avenues that address both motor and cognitive dysfunction. Emerging evidence suggests that psychedelic-assisted therapy, particularly with ibogaine, may offer neuroregenerative and functional benefits. This article presents a clinical series of three patients with idiopathic Parkinson’s disease who underwent a structured ibogaine protocol at New Path Clinic under the supervision of Dr. Carlos Silva, with neuropsychological evaluations by Eduardo Castillo Riedel, M.A. These cases demonstrate varying but overall promising outcomes across motor, cognitive, and emotional domains.
Introduction
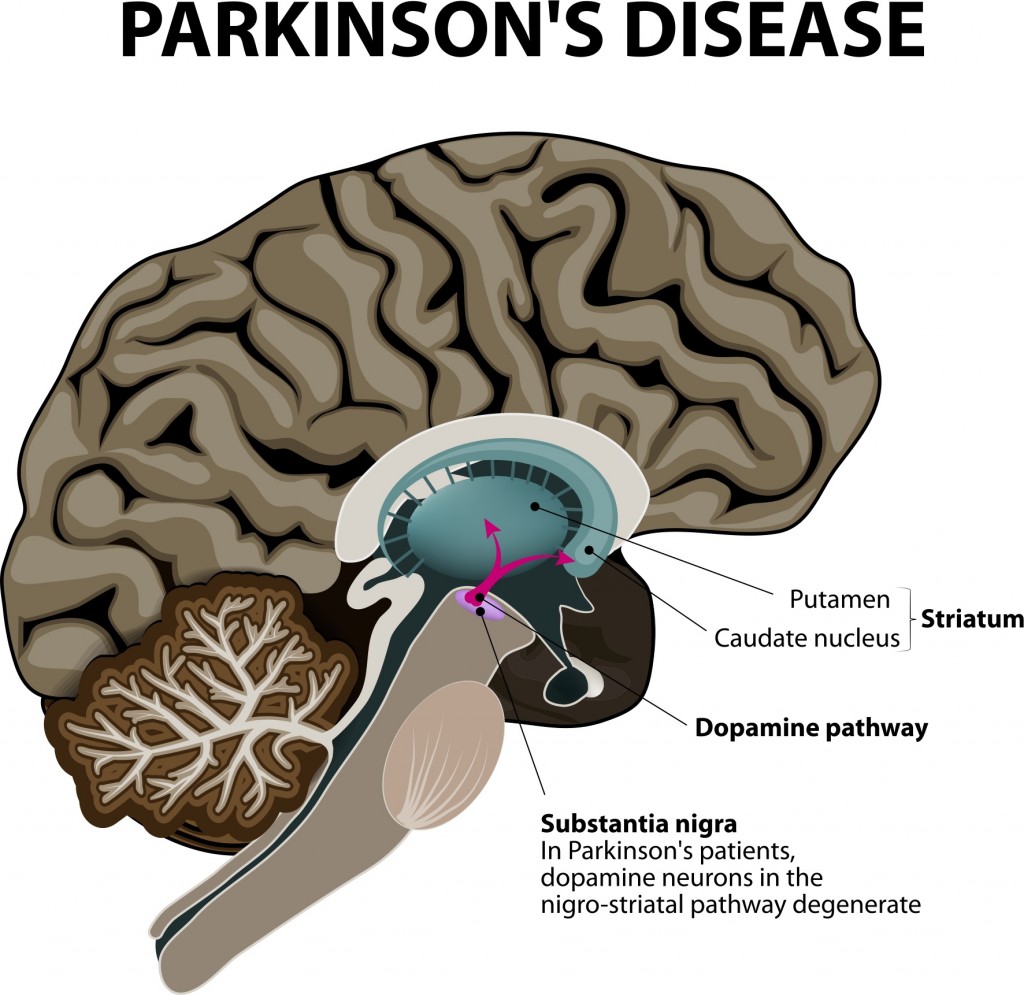
Parkinson’s disease affects over 10 million people worldwide, with symptoms ranging from bradykinesia and tremors to cognitive impairment and emotional dysregulation. Traditional pharmacological interventions offer symptomatic relief but rarely alter the trajectory of neurodegeneration. Novel treatments, including plant-based psychedelic compounds such as ibogaine, are now being studied for their potential neuroplastic and dopaminergic properties.
New Path Clinic, located in Tijuana, Mexico, has developed a multidisciplinary treatment model integrating ibogaine with medical supervision, psychotherapy, and neuropsychological follow-up. This report outlines the clinical and neurocognitive outcomes from three PD patients who underwent ibogaine therapy at the clinic between February and April 2025.
Case 1: Kevin I. (Age 53) – Restoration of Executive and Motor Function
Background
- Diagnosis: Parkinson’s disease with dominant-hand impairment
- Pre-treatment motor limitations: Unable to complete tracing or motor programming tests
- Referral motive: Neuropsychological reassessment post-treatment
Findings
Following treatment, the patient exhibited significant gains in all cognitive and motor domains. He was able to complete previously unmanageable tasks using his dominant hand, and neuropsychological testing revealed the following improvements:
| Test | Pre-Treatment | Post-Treatment | Score Change |
| MoCA | 19 | 24 | +5 |
| IFS | 13.5 | 23 | +9.5 |
| FAB | 10 | 17 | +7 |
Notably, the MIS (Memory Index Score) increased from 5/15 to 11/15. Improvements were particularly evident in spontaneous recall, executive functioning, and motor planning, as demonstrated in Luria sequences and the TMT (Trail Making Test). These changes imply enhanced connectivity between frontal-executive circuits and the motor cortex—a key dysfunction in PD.
Case 2: Jentry M. (Age 52) – Tremor Reduction and Emotional Reconnection
Background
- Diagnosis: Parkinsonism with significant upper trunk tremors
- Occupational history: U.S. military ranger and police officer
- Referral motive: Follow-up assessment of functional outcomes
Findings
Though the patient reported initial distress due to visual hallucinations during ibogaine administration, objective findings revealed substantial motor improvements:
- Tremors in the neck, eyelids, and limbs significantly reduced
- Gait, speech, arm swing, blinking, and fine motor control improved
- Social-emotional reactivation was observed: the patient began making eye contact during meals, reflecting enhanced self and interpersonal awareness
Motor exercises during neuropsychological testing, including handwriting and tracing, showed a marked reduction in involuntary movement and improved voluntary control. No cognitive decline was reported; prior scores were above clinical thresholds.
Case 3: Anonymous Male (Age 69) – Memory Recovery Despite Modest Motor Gains
Background
- Diagnosis: Parkinson’s disease (diagnosed in 2018)
- Treatment context: Perceived treatment delays, emotional disappointment regarding outcomes
- Referral motive: Follow-up cognitive and motor assessment
Findings
Although the patient perceived little change, neuropsychological testing revealed clinically significant cognitive gains, particularly in memory and recall:
| Test | Pre-Treatment | Post-Treatment | Score Change |
| MoCA | 21 | 27 | +6 |
| IFS | 20.5 | 20 | -0.5 |
| FAB | 16 | 15 | -1 |
The Memory Index Score (MIS) increased from 7/15 to 14/15, with 4 words recalled spontaneously—a dramatic shift from total dependence on recognition during baseline testing. Sleep quality improved, and freezing episodes while walking ceased, despite the patient’s subjective belief that the results were minimal.
Decreases in IFS and FAB scores were attributed to motor programming difficulties, likely due to physical symptoms rather than cognitive regression. However, abstract thinking and inhibitory control improved, suggesting better frontal lobe efficiency and cognitive flexibility.
Discussion
Across all three cases, ibogaine treatment was associated with meaningful improvements in at least one core domain: motor control, memory retrieval, cognitive fluency, or emotional self-awareness. These observations align with preclinical evidence showing ibogaine’s modulation of BDNF, GDNF, and dopaminergic signaling pathways, all of which are implicated in PD progression.
Notably:
- Two patients exhibited strong improvements in memory and executive function (MoCA gains: +5 and +6).
- All three demonstrated either motor relief (tremor reduction, gait normalization) or improvements in quality of life (social reengagement, better sleep, decreased freezing).
- The treatment appears to promote neurocognitive efficiency, enabling access to verbal fluency and spontaneous thought retrieval even when motor challenges persist.
These cases also highlight the importance of subjective experience and emotional framing. Despite cognitive and physiological improvements, patient satisfaction was partially dependent on expectations and timing of symptom change, emphasizing the need for pre-treatment psychoeducation and emotional integration support.
Conclusion
This case series provides early but compelling clinical evidence supporting the role of ibogaine-assisted therapy in the treatment of Parkinson’s disease. Under the supervision of Dr. Carlos Silva and guided by neuropsychological expertise, New Path Clinic’s integrative approach has demonstrated quantifiable benefits in memory, movement, and executive function.
Future directions include:
- Longitudinal studies on durability of cognitive gains
- Expanded clinical trials with control groups
- Development of protocols for emotional support during psychedelic experiences
For patients with Parkinson’s seeking options beyond conventional pharmacotherapy, ibogaine—administered responsibly and professionally—may represent a new frontier in neurorestorative care.
Contact & Further Reading
📍 New Path Clinic, Tijuana
🌐 www.IbogaHealth.org
📧 research@ibogahealth.org
☎️ +52-XXX-XXX-XXXX